Minoritised Ethnic Men’s Mental Health
Our 35+ year background supporting the health of local communities alongside academic literature has given us significant insight into the challenges associated with the mental health of minoritised ethnic men and the health inequalities which exist between different ethnic groups.
The need for a renewed focus in this area became increasingly apparent during our COVID-19 community engagement work when we noted that men from the Tower Hamlets Bangladeshi communities seemed to be suffering greatly. Many reported stress from loss of ‘gig economy’ jobs, or otherwise stress of a being required to keep working outside of the home when everyone else was expected to work from home. This, combined with the loss of social times at mosques and other community spaces, families being ill with COVID-19 and pressures of multi-generational families being confined at home, was leading to further emotional and mental health difficulties.
We were fortunate to secure long-term funding which allowed a multi-faceted approach to research and delivering social support groups seeking to support and improve minoritised ethnic men’s mental health whilst learning more about the challenges and realities of this issue. Our work was focused in Tower Hamlets and Hackney.
There have been four main sources of learning throughout this project:
1. Event and focus groups;
2. Social support groups;
3. Responses from a large-scale community survey of 1,065 men; and
4. Delivery reflections.
The Executive Summary and full report of our research can be found here.
Key recommendations: where do we go from here?
a) Get comfortable with being uncomfortable: It is essential for providers to be culturally aware, sensitive and open to learning be able to bring religion, faith, and culture into the conversation around mental health. Be prepared to think about your own biases and what learning / un-learning you might have to do.
b) Community Support will make the biggest improvement: If people do not identify as suffering with mental health difficulties, they will not seek support in health settings until they reach crisis point. Funding has to be in communities at grass root level to ensure there are places and people around who can support, signpost and provide services where people are, not where the system expects them to be. Ensure varied, relevant options: Intersectionality is key. No one size will fit all. We need to ensure there are plenty and varied options for mental health management that are culturally accessible to the target groups. This aspect of ‘culturally accessibility’ will vary.
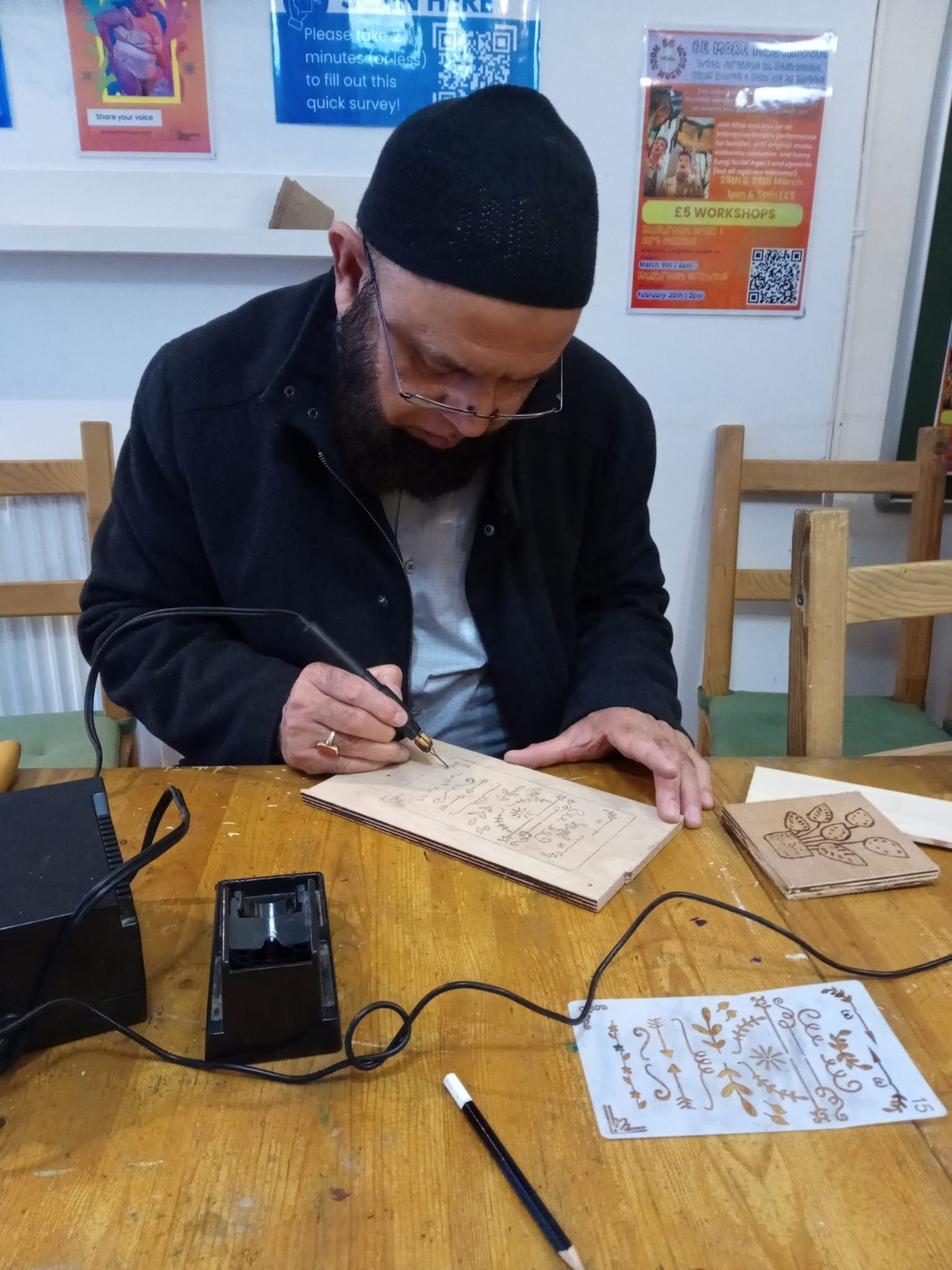
c) Start somewhere… and maybe somewhere unexpected?: The task of addressing this topic can feel overwhelming. We recommend the approach of starting somewhere and being open to change and adapting. It may be directly addressing a specific issue, or it may be something that helps someone to feel like more than the total of their issues, and feel like a person again. Can a short woodwork course improve mental health and be part of the journey of recognising mental health issues? Yes it can!
d) Support the ‘whole’ person, and the community around them: Women are carrying a disproportionate burden of supporting men with mental health difficulties. We must consider how we can support the community around men, encouraging and enabling conversations, openness and understanding that reaches homes, community spaces, and workplaces, and spans generations. We must also address mental health challenges alongside, or via, their potential root causes including social determinants of health.
e) Commit to it… long-term: In terms of engaging with the community, building trust and having a reputation for reliability is key to engaging on a large scale. Questioning our approaches and practices through this lens in all we do will make a huge difference. There are no silver bullets or quick-fixes.
f) Funding – it probably goes without saying that more funding is required. More research, more offering of activities. If we are to ensure sufficient opportunities to address poor mental health from low levels to prevent escalation to crisis support, funding needs to be long-term and consistent.
What next?
We are continuing to run groups to improve men’s mental health. Details can be found here.
We are looking for partners to work with us, fund us or to reflect and learn with us. If you would like a copy of the raw survey data on request for your own analysis, to consider partnership working or project ideas, please get in touch – email: info@safh.org.uk. It is only by working together with a joint aim of improving our communities’ health, will we make the change we all want to see.